Surgery is often the start of your treatment. Sometimes you’ll have other treatments before your surgery. The type of surgery and how much breast tissue is removed will depend on the type, size, and location of your cancer. Your surgeon will review your options with you and help you make a plan that’s right for you.
The common types of breast cancer surgery are: breast-conserving surgery, mastectomy, and mastectomy with immediate reconstruction. Most of the time these surgeries also include removing some of the lymph nodes under the arm on the same side as the breast cancer surgery.
Breast-Conserving Surgery
This type of surgery has different names: lumpectomy, segmental resection, partial mastectomy, wide excision, or a wedge resection.
For this surgery, your breast tissue with cancer is removed, along with a small amount of healthy tissue around it, called the
margin. Your incision (cut) is closed with stitches or staples. The stitches are usually dissolvable, so you won’t need them removed.
Your incision is covered with Steri-Strips® (paper tapes) and a dressing (bandage). Staples are covered with a dressing only. When your incision has healed, your doctor or nurse will remove the staples or non-dissolvable stitches.
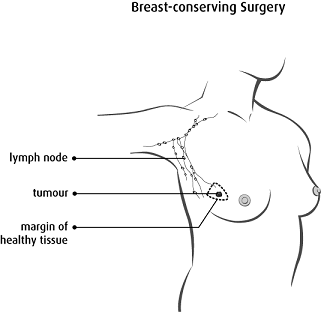
Copyright © 2017 Canadian Cancer Society. Graphic used with permission.
Margins
A pathologist will examine the tissue that has been removed to see if your margins are free of cancer. If your margins have cancer cells, it’s reported as a positive margin. If you have a positive margin,
often your surgeon will remove more tissue using the same incision site at a follow-up surgery. These results are included in your pathology report. Your surgeon will talk with you about this report at your follow-up appointment.
Mastectomy
Sometimes all of your breast tissue must be removed. This is called a mastectomy. It can be a done as a total mastectomy or a modified radical mastectomy.
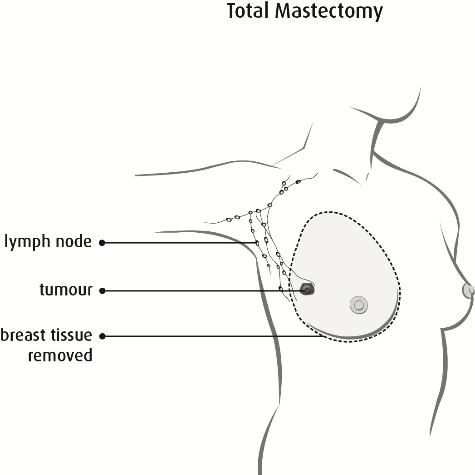
Copyright © 2017 Canadian Cancer Society. Graphic used with permission.
A total mastectomy (simple mastectomy) is when the surgeon removes all of your breast tissue. A sentinel lymph node biopsy may be included with this surgery. (See the Sentinel Lymph Node Biopsy section to learn more.)
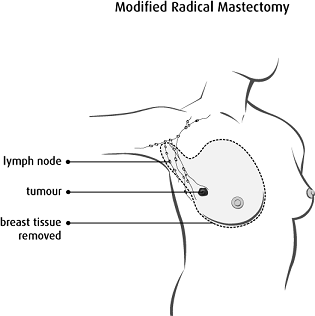
Copyright © 2017 Canadian Cancer Society. Graphic used with permission.
A modified radical mastectomy is when all of your breast tissue and the lower 2/3 of the lymph nodes in the armpit (axilla) on the same side as your breast surgery are removed.
Lymph Node Surgery
Lymph node surgery is done to see if cancer has spread to the lymph nodes and to prevent cancer from spreading in your body.
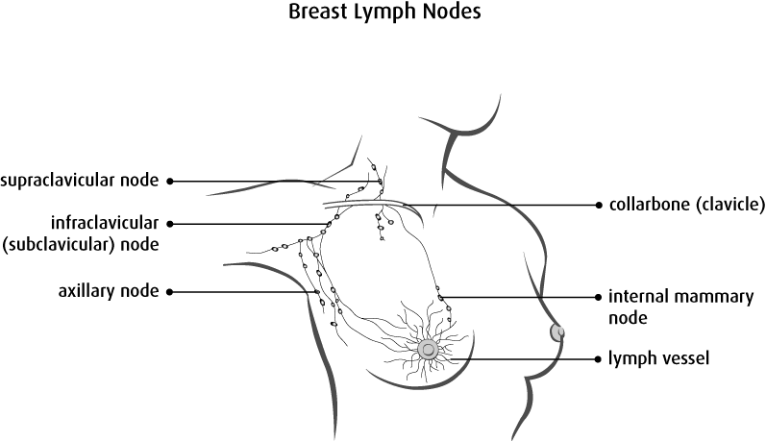
Copyright © 2017 Canadian Cancer Society. Graphic used with permission.
Lymph nodes are small glands that are found in groups throughout your body. Lymph nodes are connected by lymph vessels. Breast lymph vessels bring fluid from your breast and arm to the lymph nodes at the collarbone and armpit (axilla).
The lymph nodes filter this fluid to remove bacteria, viruses, and cancer cells. Breast cancer will most often spread to lymph nodes in your armpit before the cancer spreads to other parts of your body. There are 2 types of lymph node surgery: The
sentinel lymph node biopsy and the
axillary lymph node dissection. Your surgeon will talk to you about which surgery is right for you.
Sentinel Lymph Node Biopsy
The sentinel lymph nodes are the first nodes where breast cancer will travel as it spreads. Usually if the sentinel lymph nodes are cancer free, then it means the other axillary lymph nodes probably don’t have cancer cells.
You’ll have an appointment in the Nuclear Medicine Department or Diagnostic Imaging Centre for
Sentinel Lymph Node Mapping on the morning of or the day before your surgery. At this appointment, you’ll have a radioactive tracing material (tracer) injected into your breast near the dark skin around your nipple (areola). This tracer follows your lymph system, just as your cancer can, and provides a map of where your sentinel nodes are in your breast. The tracer doesn’t tell whether or not there is cancer in the lymph nodes. It just shows the surgeon where the lymph nodes are.
When you have your surgery, your surgeon will use a scanner to find the sentinel lymph nodes. A blue dye may be used along with the radioactive tracing material and in this circumstance, it is injected after you are asleep. The blue dye will change the sentinel nodes to a blue colour to make them easier to find. Your surgeon will remove 1 or more lymph nodes. The sentinel lymph nodes are sent to the lab where a pathologist will then test them for cancer. If the sentinel lymph nodes are cancer free, then no more lymph nodes are removed. If the sentinel nodes contain cancer cells, your surgeon
may or may not need to remove more lymph nodes. If more lymph nodes need to be removed, this is called an axillary lymph node dissection.
Some things to know:
- You may feel uncomfortable when the radioactive tracing material is injected into your breast.
- If blue dye is used, it will turn your urine (pee) green for about 24 hours. The dye may also cause the skin of your breast, where the injection was done, to turn blue. This change in colour could last for months.
- The radioactive tracing material leaves your body through your urine. It’s important to always wash your hands very well after using the bathroom. This removes any traces of radioactivity. The amount of radiation in your body is not dangerous and will disappear very quickly. You can still have contact with other people.
- Your surgeon will need all of the information about your tumour and lymph nodes before deciding if you need more surgery on your lymph nodes. The report from the pathologist can take up to 14 days.
Axillary Lymph Node Dissection
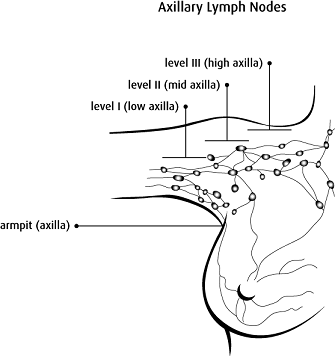
Copyright © 2017 Canadian Cancer Society. Graphic used with permission.
An axillary lymph node dissection may be done when cancer has spread extensively in the lymph nodes. If you have an axillary lymph node dissection, your surgeon will remove many lymph nodes from under your arm. Your surgeon will place a drain into the area after the lymph nodes are removed. A pathologist examines the lymph nodes for cancer cells.
The test results are reported as positive or negative for cancer. The results will help your doctors decide the stage of your cancer and the best treatment plan for you.
Breast Reconstruction Surgery
Breast reconstruction means rebuilding the breast using either breast implants or tissue from other parts of your body. Talk to your surgeon to see if breast reconstruction is right for you. If it is, you can choose whether or not to have the surgery. If you choose not to have breast reconstruction, you can always change your mind later.
Your breast reconstruction surgery will be done by one or more surgeons. In Alberta, breast reconstruction surgery is considered part of your overall breast cancer treatment. Alberta Health Care covers the cost of breast reconstruction.
You may have options for surgery. The best surgery for you will depend on:
- Your cancer site, stage, and grade.
- How much breast tissue needs to be removed.
- Your health right now.
- Your personal choice.
- Your need for other treatment after surgery, such as radiation. Reconstructive surgery is
not offered to people who smoke or have a high body mass index (BMI), because there’s a high risk of problems (complications) from surgery.
With any surgery, there are benefits and risks. Your healthcare team can help you make the best decision for you.
Breast implants
Breast implants are silicone sacs filled with either saline or silicone gel and are placed in the breast area after a mastectomy. The implant is usually placed just behind the chest muscle. If you choose to have a breast implant(s), you may first need a tissue expander put under the muscle to stretch the muscle and skin. Your surgeon will add saline to the expander every few weeks, until your skin has enough space for the breast implant. When your skin is ready, you’ll have a second surgery to remove the tissue expander and the implant will be inserted.
Some expanders are also permanent implants, so you won’t need a second surgery.
Sometimes you don’t need a tissue expander. A breast implant may be placed during your mastectomy surgery using a special mesh or your own skin to make a space under your chest muscle.
Autologous breast reconstruction (reconstructed with your own tissue)
When your surgeon uses tissue from other places in your body to recreate a breast, it’s called autologous breast reconstruction. There are many different ways a surgeon can do this. Your surgeon will talk with you about what’s right for you.
Abdominal free flap
A free flap is the most common type of autologous breast reconstruction surgery. For this surgery, your surgeon removes tissue from your abdomen (tummy area) and this tissue, called the flap, is used to reconstruct your breast. The flap is called a free flap if it’s reconnected to the blood vessels in your chest. There are several types of free flap breast surgeries:
Free TRAM flap: The free TRAM flap is done with muscle, fat, skin, and blood vessels from your abdomen.
DIEP flap: The DIEP flap is done with only fat, skin, and blood vessels from your abdomen.
These surgeries may be a better option for you than an implant, if you’ve had radiation therapy to your chest.
Pedicle TRAM flap
For the pedicle TRAM flap, your surgeon uses abdominal tissue to reconstruct the breast. The tissue stays connected to the muscles and blood vessels of the abdomen and the flap is moved under your skin to your breast area.
Latissimus dorsi or back flap
For the latissimus dorsi flap, your surgeon uses the muscle, fat, and skin from your back to reconstruct your breast. The tissue stays connected to the blood vessels and is moved under the skin to the chest area. This surgery may be right for you if you’ve had radiation treatment, you don’t have tissue from your abdomen to use, or you’ve had abdominal surgery before. You can also have a breast implant put under the flap.
