What Should I Bring to the Hospital?
- If you’ve been given a booklet copy of this information, bring it with you.
- Alberta Health Care card and your Blue Cross or other insurance card (if you have one).
- Photo ID (e.g., driver’s license, passport).
- If you live out of province, bring proof of medical coverage.
- Your medicine(s) in their original containers or a list of the medicine(s) you take and when you take them (e.g., inhalers, aspirin, vitamins, over-the-counter, and herbal medicines).
- Personal items such as hearing aids, toiletries, glasses, denture case, CPAP or BiPAP machine, housecoat and slippers (if you’re staying overnight), and walking aids such as a cane or walker.
- No more than $20 cash.
- A book or magazine to help pass the time.
Bring the items on this list in 1 small bag with your name on it. All other items can be brought to you after surgery.
Leave anything of value at home. The hospital is not responsible for lost or missing items.
Rules about using cell phones in the hospital are different on each unit. Ask your nurse before using your cell phone.
Wear comfortable clothing. You may feel uncomfortable wearing a bra right after breast conserving surgery. If you need support, you may find it helps to wear a front-opening support bra or a camisole. Have a loose-fitting button or zip-up top to wear home. Don’t wear tight-fitting or underwire bras.
Medicines
Your healthcare team will tell you what medicine you can take on the day of surgery. When you’re told this, write it down and keep it with your surgery information.
At the Hospital
When you arrive at the hospital, a nurse will:
- Go through a list of questions with you.
- Ask you to change into a hospital gown.
You may be given some medicine with a sip of water before surgery to help lower your pain and nausea.
An intravenous (IV) will be started before or when you’re in the operating room. This is a plastic tube that is placed in your vein to give you medicine and fluid during and after surgery.
You’ll be brought to an area outside of the operating room, where you’ll meet your surgical team: your anesthesiologist (the doctor who will give you medicine to keep you asleep during your surgery), surgeon, and nurses.
While you’re in the area outside of the operating room, a nurse will ask you questions from the Safe Surgery Checklist such as your name, surgery, birthdate, allergies, and what surgery you’re having. You may be asked this more than once, which is normal. Your hospital follows this Safe Surgery Checklist to keep you safe.
Waiting area
During your surgery your family and friends can wait for you in the waiting area.
The Operating room
An operating room nurse will double check your surgical information and take you into the operating room. The Safe Surgery Checklist will be repeated.
The anesthesiologist will give you medicine (general anesthetic) to make you comfortable and keep you asleep during your surgery.
Your surgery will take about 1 to 2 hours. It will take longer (2 to 7 hours) if you’re having breast reconstruction at the same time.
After Surgery
Recovery room
You’ll wake up in the recovery room after your surgery. Visitors aren’t allowed in the recovery room.
You’ll have an IV to give you fluid and medicine. You may be given medicines to help with your pain and nausea. You’ll start drinking fluids as soon as you can.
You’ll have a dressing (bandage) on your chest. It’s important not to touch your dressing to allow for proper healing.
You may have 1 or more drains near the area where the incision was made. Drains take extra fluid away from below your incision.
Your nurse will check your:
- Heart rate, breathing, blood pressure, and blood oxygen level.
- Dressing (bandage).
- Drains.
- Pain and nausea levels.
When you’ve recovered from your anesthetic, you may be taken to another unit. You’ll stay there until your healthcare team decides it’s safe for you to go home.
Managing pain and nausea
Managing pain and nausea is important. It helps you recover sooner because you will:
- Breathe and move better.
- Find it easier to eat and drink.
- Sleep better.
Pain after surgery is normal. You may have pain, numbness, or tingling in your shoulder, arm, armpit, or incision area. The type of pain you have and how long it lasts is different for everyone. Stabbing pain may happen and is normal.
You’ll get pain or nausea medicine by IV, injection, or pill as needed while you’re in the hospital. Your nurse will ask you to rate your pain and nausea from 0 (no pain) to 10 (the worst pain you can imagine). Tell your nurse when you’re having pain or nausea. The amount of pain medicine will be adjusted as needed.
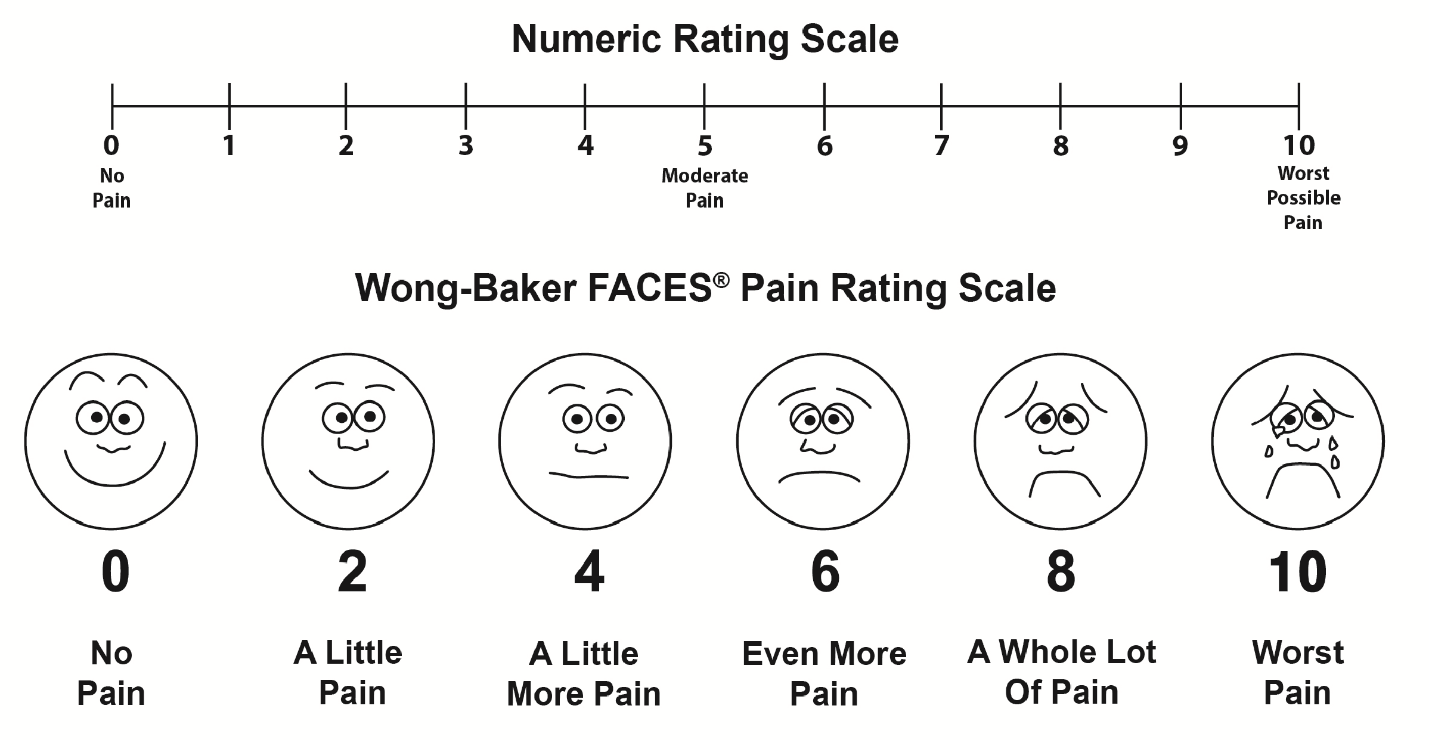
Copyright © 1983 Wong-Baker FACES Foundation. www.WongBakerFACES.org. Wording modified for adult use. Used with permission.
Eating and drinking
You can eat solid food when you are able to. Your nutrition is an important part of healing. Start with a bit of soft food and when you move to solid food, eat a nutritious, well-balanced diet. If you eat extra fibre and drink 6 to 8 glasses of water each day, it may help your bowels move regularly. If you take pain medicine this will be especially important, because some pain medicines can slow down your bowel movements (constipation).
Activity
Your nurse will help you get up and walk soon after surgery. If you take short walks, it will help you get your strength back and improve your blood flow (circulation).
Leg exercises:
When you’re awake in bed, change your position and move your legs every hour. This helps your circulation and can prevent blood clots from forming.
- Pump your ankles up and down for 1 minute, relax, and then repeat.
- Make 4 circles with your feet, first 1 way, and then the other.
- Wiggle your toes.
- Stretch your legs.
- Do these exercises at least 1 time every hour during the day. Do them 5 times each with your left leg, then 5 times each with your right leg.
Deep breathing and coughing exercises:
It’s important to do your deep breathing and coughing exercises if you have had an anesthetic. Doing exercises 1 time every hour while you’re awake will help prevent lung problems.
- Breathe in deeply through your nose.
- Hold your breath for 5 to 10 seconds, and then breathe out slowly through your mouth. You’ll find you breathe more deeply with each breath.
- Repeat again, and on the third breath in, hold your breath for 5 to 10 seconds. Cough 2 or 3 times in a row as you get rid of this breath.
- Make sure you take normal breaths when you’re not doing these exercises.
- Ask your healthcare team how often you should do these exercises.
After surgery, try to use your arm on the side of your surgery as you normally would (e.g., eating, drinking, brushing your teeth and hair, answering the phone).
Ask your doctor or nurse when you may have a shower.
Dressings and incisions
The size of your incision and where it is will depend on where your cancer was and the type of breast surgery you had. You may have a breast incision and an underarm incision.
At first, you’ll have an outer gauze dressing (bandage) covering the incisions. Gauze dressings usually stay on for 24 to 48 hours. Your surgeon will tell you when you can take your dressing off.
Your incisions are held together with staples or stitches and covered with Steri-Strips (paper or surgical tapes). The surgeon will tell you when your Steri-Strips can be removed. Dissolving stitches are used most often and don’t need to be removed.
If you have a clear, sticky dressing, it will stay on for 2 to 7 days. Your surgeon will tell you when you can take it off.
Drains
After breast surgery, it‘s normal for your body to make extra fluid in the area around your incision. You may have 1 or 2 drains that use gentle suction to remove this fluid and blood.
Removing the fluid helps with healing and lowers the risk of infection. Not everyone needs a drain.
A drain is a small plastic tube inserted through the skin near the incision. It’s stitched in place so it doesn’t fall out. A small plastic suction container is attached to it.
The drains most commonly used are the Jackson-Pratt® and the Blake®. Your healthcare team can tell you what kind of drain you have. They’ll teach you how to care for the drain at home before you leave the hospital.
For more information on how to care for your drain at home, see the At Home section.
Going Home (Discharge) Checklist
Before you’re sent home, your healthcare team will:
- Review your discharge instructions with you.
- Give you the date for your follow-up appointment
or tell you when to call your surgeon’s office to make your follow-up appointment.
- Give you prescriptions for medicines to take at home and instructions on when you can take your regular medicines.
- Ask you if you have arranged for someone to drive you home and stay with you for 24 hours after your surgery.
- Make a referral to home care if needed. Most people don’t need home care.
Talk to your healthcare team if you feel something on this list hasn’t been done.
