Preventing Diabetic Ketoacidosis (DKA) in Insulin Pump Therapy
Care instructions for children and youth
Diabetic ketoacidosis (DKA) happens when your body does not have enough insulin and your blood glucose (sugar) rises quickly. If your body cannot use glucose for energy, it uses fat for energy instead. When this happens, ketones start to build up in your blood. Higher levels of ketones in your blood can make your blood acidic, which can make you very sick and cause coma or death.
Symptoms of DKA
- breath that smells or tastes fruity
- pain in your belly (abdomen)
- nausea or vomiting
- trouble breathing or shortness of breath
- lightheadedness
- fast heartbeat
- weakness
Causes of DKA
When you use an insulin pump, you are at a higher risk for DKA because you are not using long-acting insulin.
Ketones and DKA can develop quickly (in just 2 to 4 hours) if your insulin delivery is interrupted for any of these reasons:
- infusion site failure
- missed insulin boluses
- insulin pump not working
- incorrectly stored or expired insulin
- stress
- infection, injury, or surgery
- illness (like a cold, flu, nausea, vomiting, or diarrhea)
Preventing DKA on an insulin pump
There are things you can do every day to prevent DKA:
- Check for ketones using a fingertip blood test or urine test if you have:
- glucose values over 14.0 mmol/L
- any symptoms of DKA, even if your glucose level is in target range.
- signs of dehydration, like a dry mouth, dry tongue, cracked lips, sunken eyes, drowsiness, dizziness, feeling faint, or a fast, pounding heartbeat.
- Check your glucose often throughout the day and always before bed. Consider using continuous glucose monitor high alerts.
- Inspect your pump, infusion site, insulin cartridge, and tubing and connections before bed or anytime your glucose is unexpectedly above your target range.
- Change infusion sets every 2 to 3 days or sooner, if needed. You can use extended wear infusion sets for up to 7 days.
- Rotate your infusion sites to prevent lipohypertrophy (fatty tissue lumps und the skin).
You can also prepare in advance to have the supplies and information you need to prevent DKA:
- Keep a pump safety kit available. You pump safety kit should have fresh insulin, a syringe or insulin pen, ketone testing supplies, glucose tablets, fresh batteries or power source, a blood glucose meter with test strips, and an updated list of pump settings. Fresh insulin can stay at room temperature for up to 1 month.
- Have your diabetes clinic's guidelines for managing sick days available. This may include increasing the size of boluses or using temporary increased basal rates.
- Know your diabetes clinic's guidelines for how to replace insulin if your pump fails.
- Write down your diabetes clinic's phone number or store it in your phone's contact list so it is easy to find if you need help.
- Write down the 24-hour phone number of your pump company.
Correcting high glucose and ketones on a pump
If you use an automated insulin delivery pump or hybrid closed loop pump, put your insulin pump into manual mode (if it is not already) before giving insulin with syringe or pen. Stay in manual mode for at least 4 hours after the last injection by syringe or pen. Do not use an automated insulin delivery feature (loop) during those 4 hours.
Follow the steps below to manage your high glucose and ketones.
If you have: - blood ketones 0.5 mmol/L or less
- urine ketones negative or trace (0.5mmol/L or less, or 5 mg/dL or less)
| If you have: - blood ketones 0.6 mmol/L and above
- urine ketones above trace (0.6 mmol/L or 6 mg/dL and above)
|
- Take your usual correction bolus with your pump.
- Drink 60 mL to 250 mL (1/4 cup to 1 cup) of sugar-free fluids every hour.
- Check your measurements and supplies for causes of ketones:
- Verify your sensor glucose readings with a fingertip blood glucose meter.
- Check the infusion set is attached, not leaking, and has been changed according to your clinic or manufacturer’s recommendations.
- Check the infusion site is not irritated or damp (tunneling).
- Check tubing for blood, leaks, or large bubbles. Check that you primed the tubing.
- Check your bolus history, basal rate settings, and temporary basal rates to evaluate normal pump functioning.
- Consider using a new vial or batch of insulin and change the cartridge or pod.
- After 2 hours, recheck blood glucose.
- If your glucose is below 14.0 mmol/L, give bolus correction with your pump (as recommended by the pump) every 4 hours until glucose is in target.
- If your glucose is above 14.0 mmol/L, check your ketones again.
- If your ketones areabovetrace, follow the “urine ketones above trace” steps on the other side of this table.
- If your ketones are negative or trace, correct again using a pen or syringe. Put your pump in manual mode. Change your infusion set, reservoir, tubing, infusion site, and insulin. Follow the troubleshooting steps in #3 above and recheck your blood glucose in 2 hours.
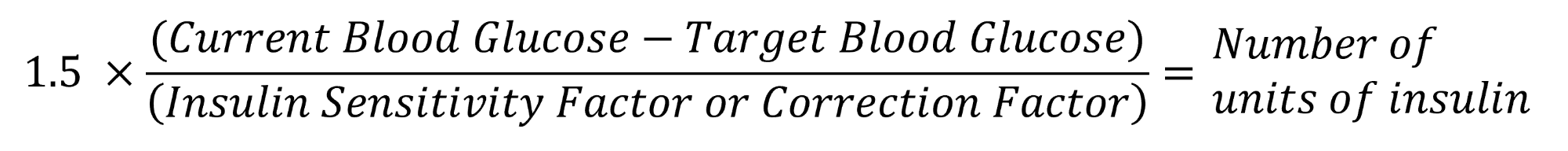
| - Take 1.5X correction of insulin by pen or syringe using these steps:
- Take your current glucose reading and subtract your target glucose reading.
- Divide this number by your insulin sensitivity factor or correction factor.
- Multiply by 1.5.
- The answer is the units of insulin to give.
- You can also do these steps as this calculation (see below the table).
- Change your infusion set, reservoir, tubing, infusion site, and insulin. Put your pump in manual mode.
- Drink 60 mL to 250 mL (1/4 cup to 1 cup) of sugar-free fluids every hour.
- Check your measurements and supplies for causes of ketones:
- Verify your sensor glucose readings with a fingertip blood glucose meter.
- Check the infusion set is attached, not leaking, and has been changed according to your clinic or manufacturer’s recommendations.
- Check the infusion site is not irritated or damp (tunneling).
- Check tubing for blood, leaks, or large bubbles. Check that you primed the tubing.
- Check your bolus history, basal rate settings, and temporary basal rates to evaluate normal pump functioning.
- Consider using a new vial or batch of insulin and change the cartridge or pod.
- After 2 hours, recheck blood glucose.
- If your blood glucose is 14.0 mmol/L or less, give bolus corrections with your pump every 2 hours until glucose is in target.
- If your blood glucose is above 14.0 mmol/L, retest for ketones and repeat steps 1 to 5. Give insulin correction by pen or syringe every 4 hours.
|
If high blood glucose and ketones continue or get worse after 2 corrections or if symptoms of DKA start or do not improve, go to the emergency department.
When should I go to the emergency department?
Go to the emergency department if you have any of these:
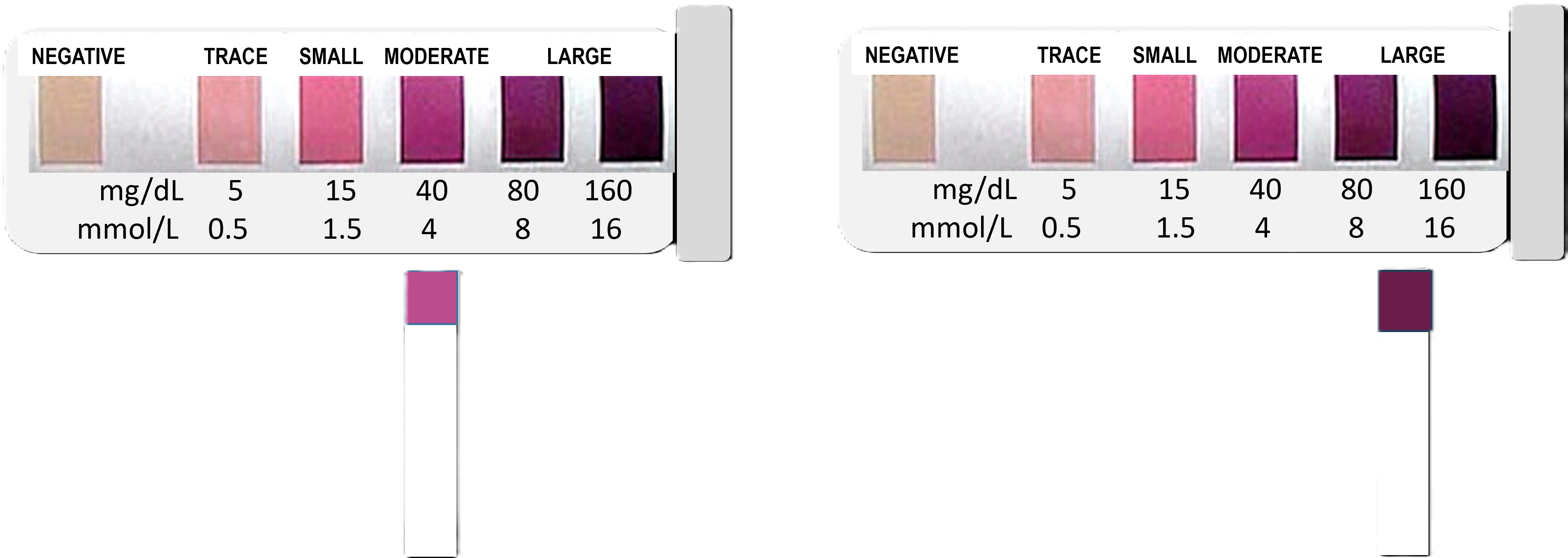
- vomiting and unable to keep fluids down and testing positive for moderate or large blood or urine ketones
- any signs or symptoms of DKA or dehydration
- high blood glucose and ketones continue or get worse after 2 corrections
- don't know how to give insulin with a pen or syringe and you can't reach your diabetes team
Examples of ketone readings
Blood ketones
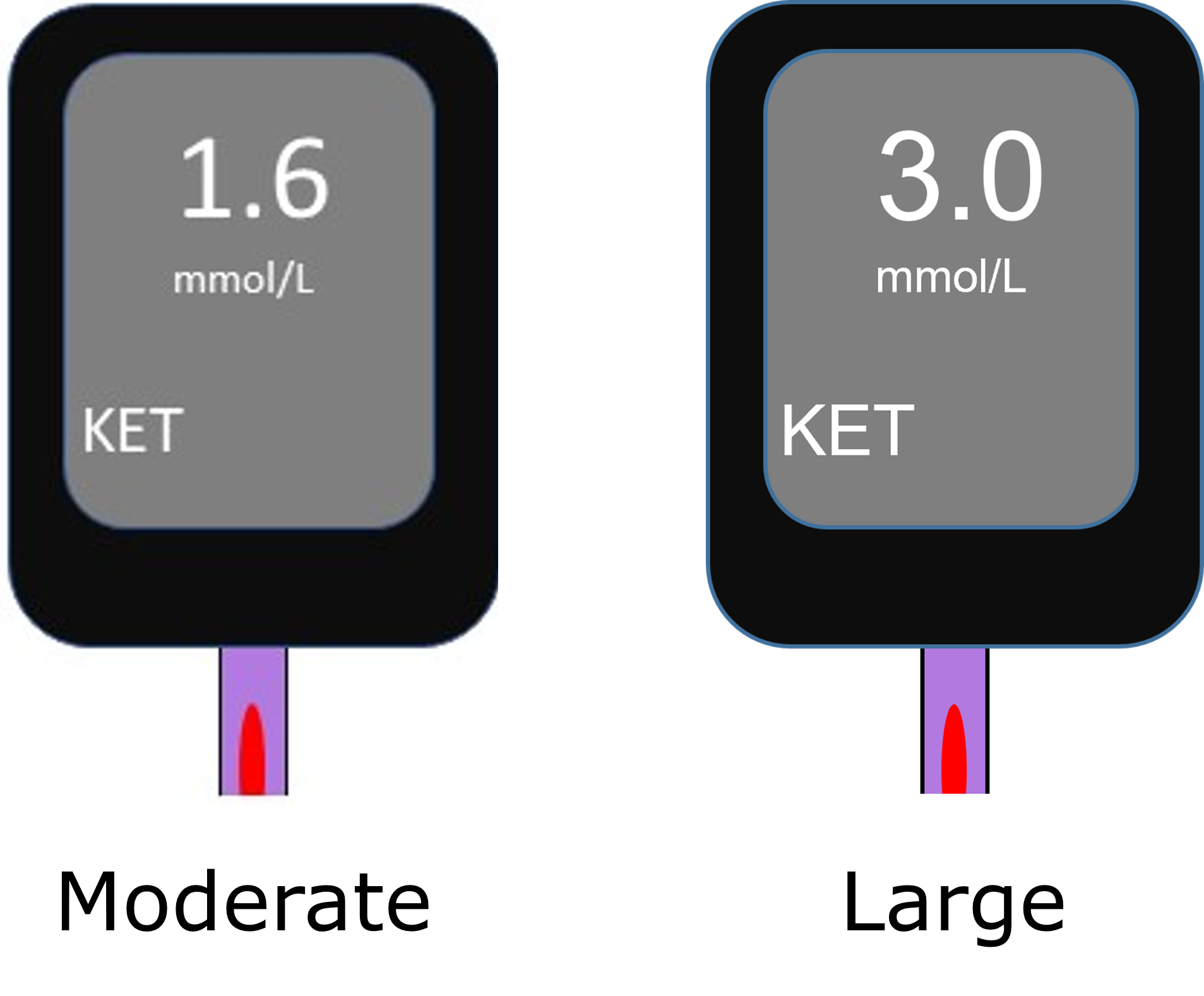
Urine ketones
Information and notes
- Diabetes centre phone number:
__________________________
- Insulin pump company phone number:
__________________________
Notes:
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
To see this information online and learn more, visit MyHealth.Alberta.ca/health/aftercareinformation/pages/conditions.aspx?hwid=custom.ab_dka_ipt_prev_child_ac.
For 24/7 nurse advice and general health information call Health Link at 811.
Current as of: August 15, 2025
Author: Diabetes, Obesity, and Nutrition Strategic Clinical Network, Alberta Health Services
This material is not a substitute for the advice of a qualified health professional. This material is intended for general information only and is provided on an "as is", "where is" basis. Although reasonable efforts were made to confirm the accuracy of the information, Alberta Health Services does not make any representation or warranty, express, implied or statutory, as to the accuracy, reliability, completeness, applicability or fitness for a particular purpose of such information. Alberta Health Services expressly disclaims all liability for the use of these materials, and for any claims, actions, demands or suits arising from such use.
