Medicines can be used to help manage the symptoms of IC/PBS, but they don’t cure the condition.
Medicines are used to help:
- control your symptoms
- keep your bladder working well and improve how well it works
- reduce the number of side effects
- reduce the number of flare-ups
All medicines will work better if you use them with:
- self-management strategies (finding ways manage the symptoms on your own)
- physiotherapy
- an exercise program
- eating healthy food
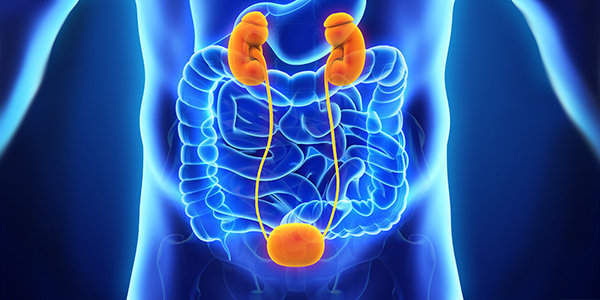
If the medicines and treatments don’t help, some people will have their bladder removed and their urine rerouted from their kidneys to the abdominal wall. If you have questions, talk to your healthcare provider.
Medicines can either be placed directly in the bladder (instillation) or taken orally (by mouth).
Bladder Instillations
During a bladder instillation, a catheter (tube) will be put into your bladder (this is called catheterization). Medicines will then be passed through the tube into your bladder.
The medicines can help with:
- pain
- an overactive bladder (feeling like you suddenly have to urinate or going often)
- improving the health of the lining of your bladder
Usually, a few different medicines (called a cocktail) are used to help with your symptoms.
You and your healthcare team will watch to see how well the treatment worked. How often the treatment needs to be repeated depends on how you feel.
Bladder instillations usually need to be done in a hospital or clinic. If you can learn how to do clean catheterizations, then prescriptions of the medicines in prefilled syringes can be used at home.
The table below shows how many medicines have been tried in treating IC/PBS. A randomized control trial is a study where using medicine is compared to not using medicine. It’s considered the best type of study to know if a medicine can help. The highlighted medicines are those recommended by the American Urologic Association guidelines.
| Silver nitrate | 60 | No |
| Clorpactin WCS-90 | 60 | No |
| DMSO | 70 | Yes |
| Bacillum Calmette-Guerin | No proven efficacy | Yes |
| Hyaluronic acid | Proven efficacy | Yes |
| Heparin | 60 | Yes |
| Chondroitin sulfate | 33 | No |
| Lidocaine | 65 | Yes |
| Capsaicin | Demonstrated efficacy | No |
| Oxybutinin | Efficacy suggested | No |
| Doxorubicin | Anecdotal efficacy | No |
| Pentosanpolysulfate | 40 | Yes |
| Bupivacaine | 66 | No |
| Hydrocortisone or Triamcinolone | Not used as a single agent | No |
(Modified from 3rd International Consultation Incontinence 2005)
There’s no correct answer to which medicine is best for you. Instillations are made just for you based on:
- your symptoms
- your bladder mucosa
- if you can get to a hospital out-patient department
- how long your symptoms need to be controlled
- if you’re able to do home instillations
Talk with your doctor about the best choice for you.
Hydrodistention
During hydrodistention, your bladder is filled with fluid and then emptied. Some people get relief for a period of time, although it’s not known how it works. To have hydrodistention, you need either general anesthetic (medicine to make you unconscious so you feel no pain) or spinal anesthetic (medicine that numbs the nerves from your waist down so you won’t feel pain).
Botulinum
The botulinum toxin is used in the cosmetic industry to treat wrinkles. It may help people with an overactive bladder and people with IC/PBS.
The toxin works in 2 ways. First, it “paralyzes” the bladder for a short time. This makes your bladder able to hold more urine so you will not need to go as often. Second, it can also affect the pain signals coming from your bladder so you may be more comfortable.
The botulinum toxin is injected directly into the bladder muscle. The treatment should work for at least 3 months. There’s a small risk that the bladder won’t empty completely after treatment. You might need to catheterize yourself to empty your bladder until the toxin wears off. It isn’t known if all the effects are truly reversible. Talk to your doctor to see if this treatment is right for you.
Oral Medicines
Medicines you take by mouth work differently than instillations.
Neuromodulation medicines work by changing some of the signals sent from your bladder to your brain. These medicines help to “turn down” the signals. They can’t completely shut down all the signals, but they can help improve your quality of life.
Some types of neuromodulation medicines include:
-
Amitriptyline—originally made to be an antidepressant, but it’s rarely used as one today. It helps with pain in people who have IC/PBS. Other antidepressants might also help with pain, although they haven’t been studied for IC/PBS yet.
-
Gabapentin and
pregabalin have been used for epilepsy but help with pain.
-
Duloxetine is good at reducing pain. It’s also an antidepressant.
There are many more medicines that seem to decrease pain although they were first used for other reasons.
Some other types of oral medicines that help with IC/PBS include:
-
Pentosan polysulfate—it protects your bladder wall from irritants in your urine. It takes 3 to 6 months to work.
-
Hydroxyzine—an antihistamine (a medicine used to treat allergy symptoms). It can help stop cells from releasing histamine, which can irritate the bladder.
-
Anticholinergics and
Mirabegron—can help treat overactive bladder, so you don’t need to pee as often or as urgently.
Talk with your doctor about these oral medicines and if they’re right for you.

Electrical Neuromodulation
This treatment involves placing electrical wires next to the nerves that go to the pelvic area near the sacrum (the bone at the bottom of your spine). The wires are attached to a battery that is placed under the skin in the buttock area (the same area you would put a wallet into a back pocket).
The wires send a constant electric signal to the nerves. If this treatment works, it can help your bladder work better and help with pain.
This may be the last option before removing or rerouting urine from the bladder.
Complementary and Alternative Medicines (CAMS)
It’s common to try alternative therapies to treat IC/PBS. Remember that many CAMS haven’t been studied and there’s no proof that they work.
People may believe that because something is natural, homeopathic, or doesn’t need a prescription, it’s safe. This isn’t always true. Talk to a doctor or pharmacist before you start any treatment. It might interact with some of your other medicines.
Below are some common CAMS that have been tried. The information was gathered from a long and detailed review.
(Source: Leong, F. C. (2014). Complementary and alternative medications for chronic pelvic pain. Obstetrics and gynecology clinics of North America, 41(3), 503-510.).
Dietary changes
Up to 90% of people with IC/PBS know of a food that makes their symptoms worse. This is the first step to
managing IC/PBS with diet.
Supplements
Some people get relief from taking
calcium glycerophosphate before meals. Check with your doctor or pharmacist to see if it will affect other medicines you take.
Up to half of people with IC/PBS say
CystoProtek improves their symptoms. It’s hard to find CystoProtek in Canada.
Quercetin is an anti-inflammatory found in red wine, green tea, and onions (foods that often make symptoms worse). It’s also found in the compound Cysta-Q (Farr Labs). There isn’t enough evidence to say that it helps, but there are many individual reports of its use. Check with your pharmacist for compounds that contain quercetin.
No studies support using
marshmallow root for IC/PBS. It’s widely recommended by people on the internet.
Recent studies on men seem to show some improvement when using
pollen extract. If you come across any other remedies, be aware of the lack of evidence that they work. Talk with your doctor before trying them.

Talk with your doctor about which medicines might help you. Ask about side effects and possible reasons why they may or may not be right for you.
There is new research and information being done on IC/PBS. New treatments may become available.
For More information on IC/PBS medicines, please visit the
Interstitial Cystitis Network or
Interstitial Cystitis Association.