Managing Pain after Surgery
You can expect to have pain after surgery, even if you’ve been given medicine for pain. It’s important that your pain is well managed so that you can stand, walk, and start your physical therapy.
How You Can Help Manage Your Pain
Tell the nurse when you’re feeling pain and ask for pain medicine. If possible, take pain medicine 30 to 45 minutes before your physical therapy sessions, so it has time to work.
| Make sure to tell your nurse about any pain medicine you were taking before surgery. |
Tell your surgeon or nurse if the pain medicine isn’t managing your pain or if you think you’re having side effects.
Ask for ice to put on your knee and for pillows to keep your operated leg raised to help lower the pain and swelling.
Pain Scale
You’ll be asked to rate your pain level using this scale. The number you choose helps your nurse or surgeon know how well the pain medicine is working for you.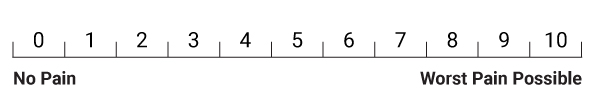
|
Tell your nurse if your pain reaches a 4 or isn’t being helped by the medicine. Don’t wait until the pain is bad. |
Deep Breathing, Coughing, and Moving after Surgery
You’ll have to breathe deeply and cough at least once an hour after surgery to clear your lungs.
You’ll be shown foot and ankle exercises to do once every hour to help prevent blood clots.
Preventing Blood Clots
You’ll need to take a blood thinner after surgery to lower the chance of getting a blood clot. Your surgeon will decide how long you should be on a blood thinner. You’ll be given a prescription for a blood thinner to take for a few weeks after you go home. If the blood thinner is given by needle, your nurse will show you how give the injection before you leave the hospital.
Replacing Blood Lost during Surgery
Everyone loses blood during knee replacement surgery. Losing too much blood may leave you feeling dizzy, tired, short of breath, sick to your stomach, and you may have a headache.
Losing too much blood can slow your healing and recovery. Your surgeon may start you on iron pills or give you a blood transfusion to build up your blood levels.
Diet
It’s important to eat healthy foods and drink lots of fluids after your surgery.
After surgery, you’ll get fluids by IV until you can eat and drink enough on your own.
Once you’re able to eat and drink, you can start eating your regular diet. Follow the guidelines in
Canada’s Food Guide. If you aren’t eating well, ask your healthcare team about taking a nutrition supplement.
Healthy eating after surgery helps you feel better sooner because it:
- helps repair muscles and tissues
- builds up the iron in your blood
- gives you the strength and energy to do activities
Managing Your Bathroom Needs
To prevent constipation:
- drink at least 8 cups (2 litres) of water every day
- eat foods with fibre
- walk
- do your exercises every day
If you’re constipated, a nurse will offer you something to help your stools pass. It’s important to tell the nurse when you’ve had a bowel movement.
If a tube was inserted to drain your urine during and after surgery, it will be taken out the morning after surgery. The nurses will make sure you can urinate (pass water) without the tube.
Washing, Brushing, and Other Personal Needs
You’ll be expected to do your personal hygiene on your own. Please ask your nurse if you need help. Make sure all the items you need are within reach before you start.
You’ll be allowed to shower after the bandages around the area of surgery are changed for the first time or when your surgeon tells you it’s okay to shower. Don’t put any lotions or creams on your operated leg for the first 6 weeks after surgery.
Rest and Activity
You need both rest and activity to recover. You’ll tire easily the first few weeks after surgery. You may find that your normal sleep patterns also change. Let the way you feel be your guide to what you can and can’t do.
Stop what you’re doing and rest when you begin to feel tired. It’s better for you to do shorter activities (like walking) more often, rather than doing one long activity. Remember to do your foot and ankle exercises every hour.
Leg Swelling
Your leg will swell as you become more active after surgery. It’s normal for your knee to be warm and swollen for many weeks after surgery.
- To control the swelling, don’t sit for more than 30 minutes at a time.
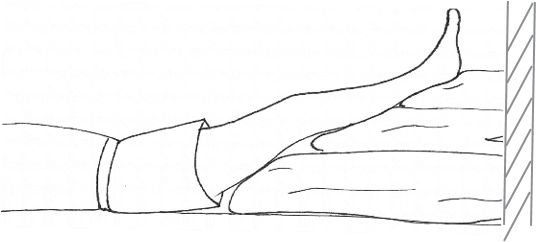
- Lie on your back, with your operated leg resting on pillows so that your foot is above the level of your heart.
Keep your leg as straight as you can. Make sure the pillow isn’t under the back of your knee. Raise your operated leg this way 2 to 3 times a day for 45 minutes each time.
- Put a cold pack on warm or swollen areas after you’re done your exercises. Use crushed ice in a bag, an instant cold pack, or a bag of frozen peas or corn. Make sure you have a thin towel between your skin and the cold pack to protect your skin. Don’t leave the cold pack in one place for more than 20 minutes at a time.
|
Tell your nurse or surgeon right away if you have pain in your calf or chest. |
Rehabilitation
You’ll be helped to move from your bed to a chair. You may be standing and walking within 4 to 8 hours after surgery. Your activity level will go up every day. You’ll also begin a program to help improve the flexibility or range of movement in your new knee and make the knee stronger.
- Most people are allowed to put as much weight on the operative leg as they can tolerate. Your healthcare team will let you know if your surgeon wants to limit the amount of weight you can put on the operated leg.
- Your physical therapist will teach you to use a walker. You’ll also be shown the exercises you must do.
Use your walking aid until your surgeon or physical therapist says you can stop.
- Your healthcare team will check how well you can do the exercises on your own and move around. They will also see if you have the skills you need to manage at home. The team will use the results to recommend when you should leave the hospital and what community services you may need at home.
